Scientists say they are closer than ever to growing human eggs from body tissue. At George Church’s lab at the Wyss Institute of Harvard, researchers say this process could open up reproductive options for people who cannot naturally produce their own eggs. Merrick Pierson Smela, a graduate student in Church’s lab and one of the leaders of the study, joins All Things Considered host Arun Rath to elaborate. The following transcript has been lightly edited.
Rath: As we look at this as a process and an aid to human reproduction, what is different about this process from typical in vitro fertilization? How does this change human reproduction?
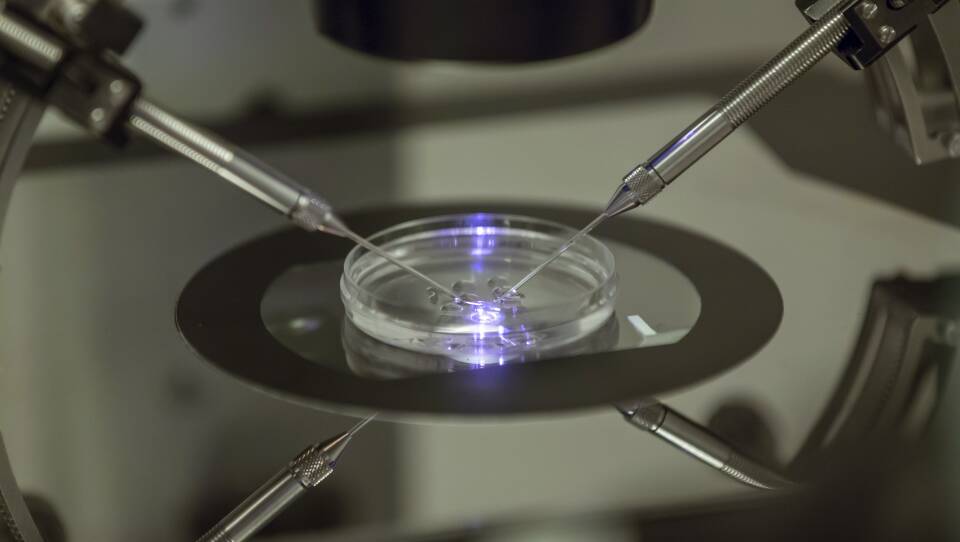
Smela: With in vitro fertilization, you need to stimulate the ovaries to produce or release eggs and then collect them from the woman. Then, you can use them for fertilization and implantation of the resulting embryos.
With this, you basically outsource the ovary to cell culture. You would take a skin or other cell tissue biopsy, reprogram those cells into stem cells, grow eggs from those stem cells, and use that instead of eggs you isolate from a woman’s ovaries.
So it’s a similar end process to IVF, but the way you get the eggs would be different.
The approach that we have taken to generate these ovarian-supporting cells was somewhat different, technically, than the previous approach. Basically, the previous approach tried to mimic the natural signaling environment of the developing ovary by adding signaling proteins to the culture medium. Instead, we expressed transcription factors, which are basically genes that control the expression of other genes. So by turning on particular transcription factors, we can tell the cells to become ovarian-supporting cells.
The other half of the organoids are these things called germ cells, which are basically early precursors for eggs or sperm. We can generate those by a signaling, protein-based approach. This has been known in the literature for a few years now. When we combined these germ cells with the ovarian-supporting cells that we made, encouragingly, the germ cells seem to develop to a bit of a later developmental stage than they started out as. They’re not going all the way to eggs yet, but we’re working on having improved culture systems that could potentially do that.
Rath: When you’re starting off with these stem cells, does it have to be female DNA to create an egg cell?
Smela: So if you have a Y chromosome, you’re going to run into trouble with making eggs. The thing is, though, that it is possible for researchers to take a male cell — which has X and Y chromosomes — get rid of the Y chromosome, and duplicate the X chromosome. In a study published last March, this was performed in mouse cells generating mouse eggs from originally male cells. So the answer is you can’t do it directly, but there could be ways to get around that barrier and generate eggs from men.
I will say, though, that if you’re planning to use this for human reproduction, there are extensive safety studies that will need to be performed before anyone can think about actually using this.
Rath: Let’s talk about that. First off, what would be the ultimate goal with this to be used for reproductive health or IV fertilization or that kind of thing?
Smela: Yeah. So basically, the overall plan or dream would be to be able to grow eggs from anybody who wants their own eggs, even if they can’t produce them naturally, or they’re too old, or things like that.
Of course, as I mentioned, there are definitely lots of safety concerns. If you have improper epigenetics of the eggs or sperm that you’re producing, the offspring will not develop normally. This can be seen even in the mouse studies that have been done: only 1% or so of the eggs that they produce are actually able to develop into live mice after fertilization. So, clearly, there are some quality issues with the approach of growing them in cell culture as it is currently.
Rath: You talked about some of the safety aspects that need to be figured out along the way. I have to think that there are probably ethical concerns. Tell us about the ethical framework that you have to consider as you’re doing this kind of research.
Smela: I mean, obviously, you want to respect everybody’s autonomy, and you don’t want to inflict suffering that is unjustified. You want to be sure that the children that would come out of this are healthy.
I also am interested in making sure that this technology is not restricted to only a certain rich group of people who are the only ones able to afford it because it’s so expensive. Hopefully, it will become more broadly accessible, and it won’t lead to reproductive inequalities.
Rath: Is that something like, in the popular mind, might be things like "designer babies," so-called, things that people would do to get a genetic advantage?
Smela: This technology is different from gene editing or embryo selection. I think that those other technologies would be the focus of regulation. This one is basically just expanding the set of people who are able to have biological children.
Rath: It sounds like there is a lot to figure out before we would get to that point where people could have healthy human children this way. Do you have any sense of how long that might take?
Smela: I think we will likely see the first proof-of-concept example of a human egg being produced within probably one to two years. I think there are a lot of researchers who are working on this, and it’s moving along pretty quickly.
In terms of the actual use of this for human reproduction, I think that it will depend a lot on the safety and regulatory aspects. I would be very surprised if it was within 10 years — I would say probably 20 years is a good estimate.
For safety, I would want to see this research done in a few species of animals, and particularly other primates besides humans. For those sorts of studies, you need to wait a few years to see if the babies develop normally, so there’s a fundamental limit on how quickly you can take things if you want to be safe.
Rath: Right. You can’t really rush life, I guess.
Smela: Exactly.